 Indiana’s hospitals have had many challenges in recent years but remain incredibly resilient, providing world-class care to every person who walks through their doors. Indiana’s doctors, nurses, and caregivers took extraordinary action to save lives over the past two and a half years and faced the greatest hospital capacity crisis of the pandemic just a few months ago. Today, we are still providing the highest quality care to patients who are frequently sicker and need longer stays in our facilities due to care delayed because of the pandemic.
Indiana’s hospitals have had many challenges in recent years but remain incredibly resilient, providing world-class care to every person who walks through their doors. Indiana’s doctors, nurses, and caregivers took extraordinary action to save lives over the past two and a half years and faced the greatest hospital capacity crisis of the pandemic just a few months ago. Today, we are still providing the highest quality care to patients who are frequently sicker and need longer stays in our facilities due to care delayed because of the pandemic.
While the pandemic may have subsided, hospitals continue to face significant headwinds – an unprecedented workforce crisis, skyrocketing costs of drugs, labor, and equipment, and lingering supply shortages that strain resources and threaten access to care.
Recently, Fitch Ratings described the financial status of hospitals as “deteriorating,” noting that “conditions will remain challenged for the remainder of 2022 as labor pressures and generationally elevated inflation compress margins for most providers.” Since then, we have seen large health systems announce losses of billions of dollars already this year.

Further, many community hospitals are operating in the red, which is concerning given that Indiana was recently ranked by the Center for Healthcare Quality and Payment Reform (CHQPR) as having the highest risk of hospital closures among our surrounding states. According to CHQPR, 22% of Indiana’s rural hospitals are at immediate risk of closing due to continuing financial losses and lack of financial reserves to sustain operations.
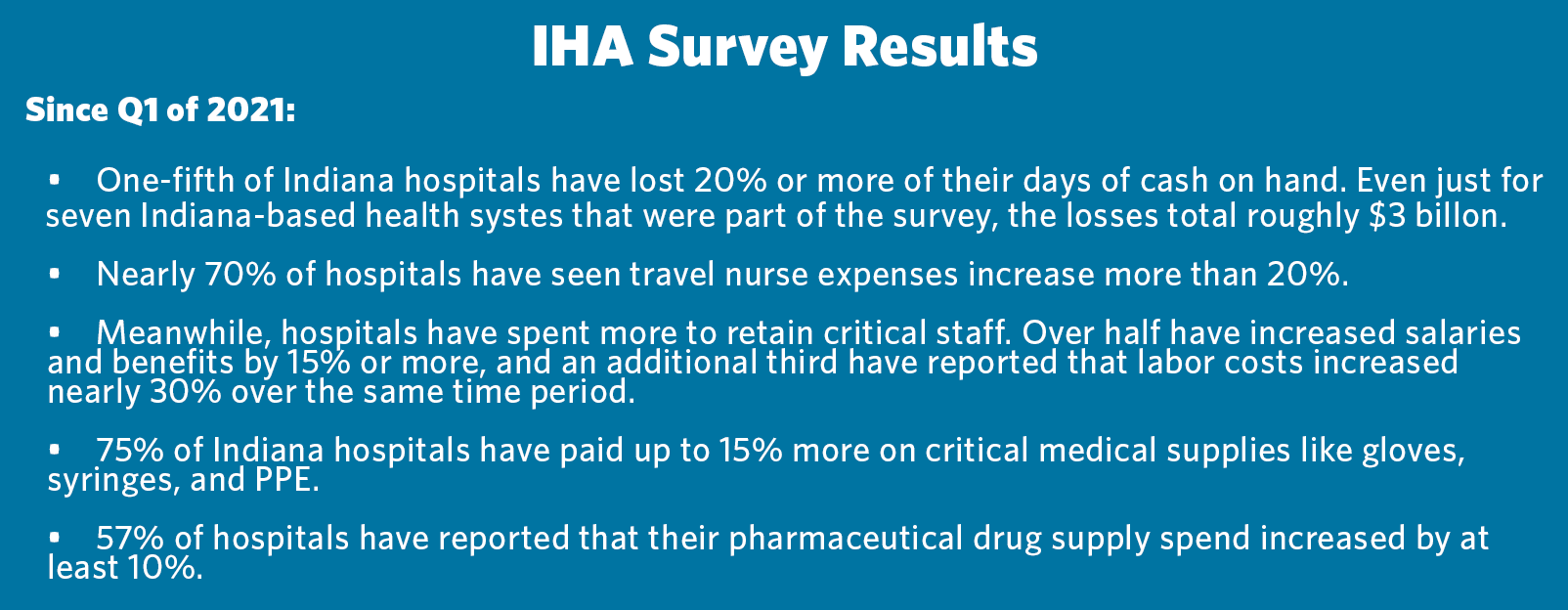
An IHA survey highlights the significant increase in costs these organizations must bear. Inflation has exacerbated these increases, resulting in widespread financial losses. These financial impacts are hitting just as hospitals are rebuilding from the highest inpatient levels in our state’s history, and they are compounded by looming reductions in government payment programs that will be especially difficult for our safety net and rural facilities to sustain.
The perfect storm is forming, as those hospitals most reliant on Medicare funding will see their funding expire at the end of this year unless renewed by Congress. In about two dozen rural communities across Indiana like New Castle, Vincennes, and Seymour, this dangerous financial cliff at the end of 2022 means further uncertainty. In addition, recent federal changes to the funding pool for high-Medicaid safety net facilities could mean that $100 million each year is now out of reach for urban hospitals in Gary and other Indiana cities.
It is broadly recognized that government programs pay hospitals far less than the cost of providing care. In Indiana, Medicare pays 87 cents on the dollar and Medicaid pays 23 cents on the dollar to hospitals based on the cost of care. The government’s own oversight body, the Medicare Payment Advisory Commission, projects that the negative margin hospitals experience in Medicare will grow in 2022.
These shortfalls are even more significant when considering how many patients are covered by one of these government programs. In Indiana, 83% of all hospitals have 67% or more of their inpatient days paid by Medicare or Medicaid. For just under half the hospitals in our state, the percentage is greater than 75%.
Taken together, these challenges are incredibly daunting for our health care system, patients, and communities. We must ensure hospitals and caregivers have the resources they need to provide access to the high-quality health care Hoosiers rely on — 24 hours a day, seven days a week.
